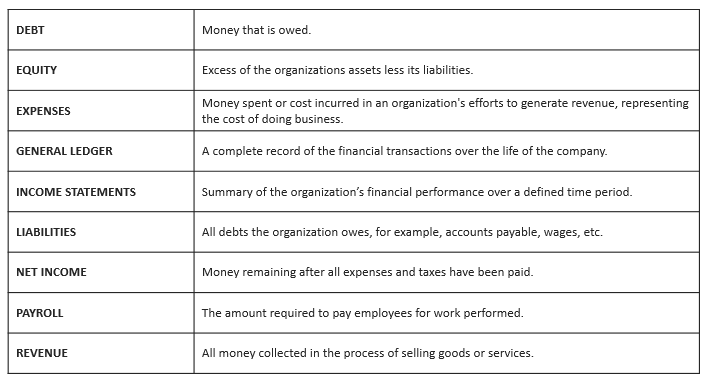
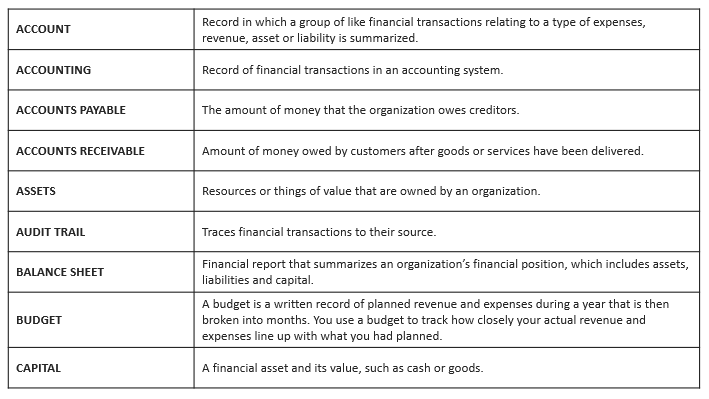
Financial Terminology
Financial Terminology
Finance Departments
The Fairview Finance Department is responsible for the functions that help shape the financial performance of the organization.
Finance at Fairview
Services Provided:
- Fairview Financial Department Teams
- Accounting
- Operations Finance
- Revenue Management
- Corporate Finance
- Tax Department
- Treasury
- Revenue Cycle

The Fairview Accounting department is responsible for recording, classifying and maintaining Fairview’s financial information and sharing that information as appropriate with stakeholders, managers and employees.
Accounting Services:
- General accounting and controls
- Cost accounting
- Accounts payable processing
Operations Finance is a business partner to operations and acts as a liaison between Operations and Finance and brings valuable insights to help leaders across the organization make informed decisions to improve the organization.
Services Provided:
- Financial liaison support to leadership
- Month-end reporting and analysis
- Dialogue and offer suggestions about how to improve financial performance
- Provide ad-hoc analysis to support decisions
- Support operations in completing financial planning
Revenue Management team is dedicated to improving the organization’s financial performance and exceeding our customers’ payer and pricing needs.
Services provided:
- Charges codes & pricing
- Government reimbursement
- Managed care/contracting
- Revenue recovery
Managed Care is a complex system of plans and organizations that integrate the financing and delivery of health care services.
Fairview Pricing assists with establishing the fees for services and supplies that are provided throughout our facilities to meet our strategic and tactical pricing plans.
Corporate Finance is in charge of the following for the System:
- Strategic analysis
- Capital planning
- Financial planning and analysis
- Operational finance for shared services
- Revenue analysis and decision support
The Tax Department is responsible for tax planning, compliance, and tax related aspects of mergers and acquisitions for the organization.
Treasury is responsible for cash/bank management, capital structure and debt compliance, short and long-term investment portfolio management, oversight of retirement plan assets, insurance/financial risk management, cash applications and overall balance sheet management. They focus on capital expenditure policies, investment policies, loan policies. Debt and equity is evaluated to determine how to use it for funding in capital investments.
Revenue Cycle – Wide range of processes to ensure our organization is paid appropriately for the services provided to the patients.
Revenue Cycle includes:
- Scheduling and registration
- Financial securitization
- Documentation
- Health Information Management and Coding
- Billing and Collections
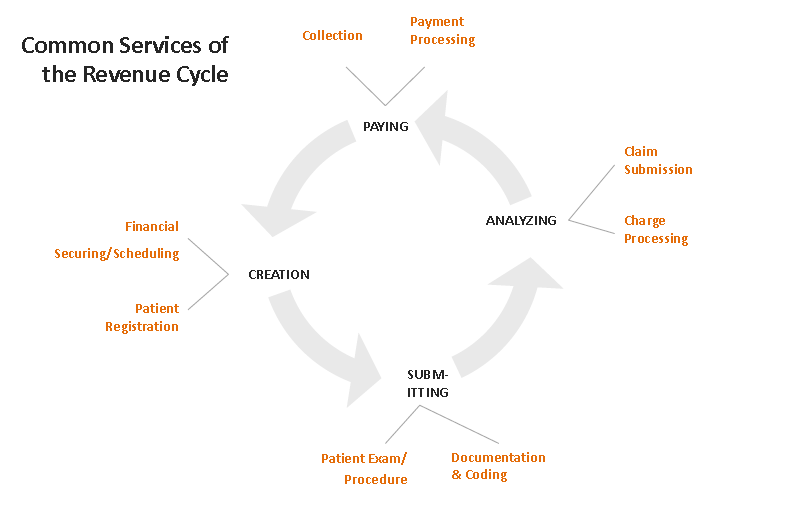
Revenue Cycle
Revenue Cycle is the financial process that relates to creating, submitting, analyzing and receiving reimbursement for clinical encounters. Revenue cycles processes flow into and affect one another. When process are correctly executed, the cycle performs quite predictably. Errors within the cycle can cause delays or negative effects.
- Revenue Cycle
- Financial Securing and Scheduling
- Patient Registration
- Patient Exam and Procedure
- Documentation and Coding
- Charge Processing
- Claim Submission
- Payment Processing
- Collection
Scheduling and Financial Securing
Assists with setting expectations about
- Wait times
- Time of procedure or results
- Medications
- Patient Instructions
- Get referral requests
•Coordinate with patient care staff
Patient Registration and Front Desk
- Confirm demographics, eligibility, benefits
- Tracks no shows and phone calls
- Patient co-pays
- Reminders for patients about wait times, medications, procedures, etc.
- Regulatory requirements
Patient Exam and Procedure
- Consider medical necessity
- Coordinate with all service providers
- Initiate care planning/discharge planning
- Utilize structured documentation to capture proper coding
- Comply with regulatory mandates
Documentation and Coding
- Review documentation to ensure it supports care rendered
- Clear, concise, complete, legible
- Consider special payorrequirements & ensure documentation or other supporting documents are present
Charge Processing
- Maintenance of Charge Master
- Charges can be added manually or automatically
- Departments are responsible for late charges
Claim Submission
Review of claims information to ensure they are complete & accurate for greatest probability of payment and to prevent denials
- Registration error correction
- Medical documentation required
- Correcting coding/errors
- Missing referrals and authorizations
Payment Processing
Billing
- Field pay or questions & requests for additional documentation in an effort to get paid
- Work with coding to correct errors
- Submit appeals
- Search for additional coverage
- Missing referrals and authorizations
Collection
- Collect patient self-pay balances
- Verify demographics
- Call patients for payments
- Payment plans
- Charity/Community Care
- Outsource to agencies
